Positive association between COVID-19 deaths and influenza vaccination rates in elderly people worldwide

- October 14, 2020:
Publisher Note: Given the public interest in articles which report on vaccination, the publisher reminds readers that correlation (which this article reports upon for a specific age group) does not necessarily equal causation.
What does that mean? By way of example, in some cities increased ice cream sales correlate with increased murder rates. But that doesn't mean that if more ice creams are sold, then murder rates will increase. There is some other factor at play - the weather temperature.
Similarly, this article should not be taken to suggest that receiving the influenza vaccination results in an increased risk of death for an individual with COVID-19 as there may be many confounding factors at play (including, for example, socioeconomic factors).
The publisher also wants to draw the attention of readers to the peer-review history of this article.
Author and article information
Abstract
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is an ongoing global health crisis, directly and indirectly impacting all spheres of human life. Some pharmacological measures have been proposed to prevent COVID-19 or reduce its severity, such as vaccinations. Previous reports indicate that influenza vaccination appears to be negatively correlated with COVID-19-associated mortality, perhaps as a result of heterologous immunity or changes in innate immunity. The understanding of such trends in correlations could prevent deaths from COVID-19 in the future. The aim of this study was therefore to analyze the association between COVID-19 related deaths and influenza vaccination rate (IVR) in elderly people worldwide.
Methods
To determine the association between COVID-19 deaths and influenza vaccination, available data sets from countries with more than 0.5 million inhabitants were analyzed (in total 39 countries). To accurately estimate the influence of IVR on COVID-19 deaths and mitigate effects of confounding variables, a sophisticated ranking of the importance of different variables was performed, including as predictor variables IVR and some potentially important geographical and socioeconomic variables as well as variables related to non-pharmaceutical intervention. The associations were measured by non-parametric Spearman rank correlation coefficients and random forest functions.
Results
The results showed a positive association between COVID-19 deaths and IVR of people ≥65 years-old. There is a significant increase in COVID-19 deaths from eastern to western regions in the world. Further exploration is needed to explain these findings, and additional work on this line of research may lead to prevention of deaths associated with COVID-19.
Cite this asWehenkel C. 2020. Positive association between COVID-19 deaths and influenza vaccination rates in elderly people worldwide. PeerJ 8:e10112 https://doi.org/10.7717/peerj.10112
Main article text
Introduction
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is an ongoing global health crisis (Yuen et al., 2020), directly and indirectly impacting all spheres of human life (Ozili & Arun, 2020). More than 31,000,000 confirmed cases including more than 970,000 deaths have been documented worldwide, affecting 213 countries and territories around the world (https://covid19.who.int/).
Determining the factors influencing the severity of COVID-19 is important (Armengaud et al., 2020). Although COVID-19 disease does not only affect elderly people, the severity of symptoms increases with age (https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html; Le Couteur, Anderson & Newman, 2020).
Several other risk factors have been found for severe COVID-19, such as comorbidities, dyspnea, chest pain, cough, expectoration, decreased lymphocytes, and increased inflammation indicators (Li et al., 2020). Low socioeconomic status is an additional risk factor (Yancy, 2020).
In response to the increasing numbers of COVID-19 cases and deaths, numerous non-pharmaceutical interventions have been implemented, including social distancing, border closures, school closures, measures to isolate symptomatic individuals and their contacts, and large-scale lockdowns of populations (Courtemanche et al., 2020; Flaxman et al., 2020). Some pharmacological measures have also (often controversially) been proposed in order to prevent COVID-19 disease or reduce its severity, such as the use of remdesivir (Beigel et al., 2020), dexamethasone (RECOVERY Collaborative Group, 2020), adjunctive therapies (https://files.covid19treatmentguidelines.nih.gov/guidelines/section/section_85.pdf) and COVID-19 candidate vaccines (Graham, 2020, https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines).
The term “heterologous immunity” is applied when an infection by one pathogen can induce and/or alter the immune response against another unrelated pathogen. Heterologous immunity can improve or decrease protective immunity against a given pathogen, and/or cause severe immunopathology or tolerance to self-antigens. Heterologous immunity can also result in non-specific effects (also called “heterologous effects”) of vaccines which affect unrelated infections and diseases, such as extending the protective outcomes of vaccinations (Goodridge et al., 2016; Agrawal, 2019). Arokiaraj (2020) reported a negative correlation between influenza vaccination rates (IVRs) and COVID-19 related mortality and morbidity. Marín-Hernández, Schwartz & Nixon (2020) also showed epidemiological evidence of an association between higher influenza vaccine uptake by elderly people and lower percentage of COVID-19 deaths in Italy. In a study analyzing 92,664 clinically and molecularly confirmed COVID-19 cases in Brazil, Fink et al. (2020) reported that patients who received a recent flu vaccine experienced on average 17% lower odds of death. Moreover, Pawlowski et al. (2020) analyzed the immunization records of 137,037 individuals who tested positive in a SARS-CoV-2 PCR. They found that polio, Hemophilus influenzae type-B, measles-mumps-rubella, varicella, pneumococcal conjugate (PCV13), geriatric flu, and hepatitis A/hepatitis B (HepA-HepB) vaccines, which had been administered in the past 1, 2, and 5 years, were associated with decreased SARS-CoV-2 infection rates.
By contrast, in a study with 6,120 subjects, Wolff (2020) reported that influenza vaccination was significantly associated with a higher risk of some other respiratory diseases, due to virus interference. In a specific examination of non-influenza viruses, the odds of coronavirus infection (but not the COVID-19 virus) in vaccinated individuals were significantly higher, when compared to unvaccinated individuals (odds ratio = 1.36).
Given that heterologous immunity could improve protective immunity against COVID-19 and, thus, prevent COVID-19 deaths in the future, the aim in this study was to analyze the possible association between COVID-19 deaths and the IVR in elderly people worldwide. A negative association was expected.
Materials and Methods
To look for an association between COVID-19 deaths and influenza vaccination, I analyzed available data sets from 39 countries, each with ≥0.5 million inhabitants. In smaller states (i.e., <0.5 million inhabitants), the rate of erroneous identification of COVID-19 deaths may be particularly high due to the lack of expertise, measuring devices and experience. Moreover, in such microstates small absolute changes in COVID-19 deaths may result in extreme values of relative indices, such as COVID-19 deaths per million inhabitants (DPMI) and COVID-19 Case Fatality Ratio (CFR).
I analyzed the variables DPMI and CFR, based on documented COVID-19 cases per million inhabitants (CPMI) in 2020, COVID-19 tests per million inhabitants, and IVR (%) in people ≥65 years old in 2019 or latest available data (Table 1). I recorded the DPMI, CPMI and CFR data from the public web site https://www.worldometers.info/coronavirus/. Then, I calculated CFR as the rate of DPMI per CPMI. IVR data were also taken from https://data.oecd.org/healthcare/influenza-vaccination-rates.htm, https://oecdcode.org/disclaimers/israel.html and https://www.statista.com/chart/16575/global-flu-immunization-rates-vary/ (retrieved on July 25, 2020). Vietnam’s 2017 IVR was recorded from Nguyen et al. (2020), and Singapore’s 2016/2017 IVR from https://www.todayonline.com/commentary/why-singapores-adult-vaccination-rate-so-low.
| Country | IVR* (%) | Year of IVR | DPMI+ (N per M) | CPMI+ (N per M) | CFR+ | COVID-19 tests+ | Continent |
|---|---|---|---|---|---|---|---|
| Australia | 73.0 | 2018/2019 | 6 | 547 | 0.011 | 151,037 | Australia and Ozeanien |
| Belgium | 59.1 | 2019 | 847 | 5,624 | 0.151 | 130,601 | Europe |
| Brazil | 71.8 | 2018/2019 | 402 | 11,078 | 0.036 | 23,094 | America |
| Canada | 59.0 | 2019 | 235 | 3,006 | 0.078 | 98,442 | America |
| Chile | 68.3 | 2019 | 472 | 17,964 | 0.026 | 78,678 | America |
| China | 7.0 | 2018/2019 | 3 | 58 | 0.052 | 62,814 | Asia |
| Croatia | 23.0 | 2017 | 31 | 1,168 | 0.027 | 26,932 | Europe |
| Czech Republic | 21.5 | 2019 | 34 | 1,413 | 0.024 | 61,332 | Europe |
| Denmark | 52.0 | 2019 | 106 | 2,319 | 0.046 | 243,677 | Europe |
| Estonia | 10.2 | 2019 | 52 | 1,532 | 0.034 | 87,692 | Europe |
| Finland | 49.5 | 2019 | 59 | 1,333 | 0.044 | 59,654 | Europe |
| France | 51.0 | 2019 | 462 | 2,765 | 0.167 | 45,683 | Europe |
| Germany | 34.8 | 2019 | 110 | 2,460 | 0.045 | 88,528 | Europe |
| Greece | 56.2 | 2019 | 19 | 400 | 0.048 | 42,244 | Europe |
| Hungary | 24.1 | 2019 | 62 | 458 | 0.135 | 33,116 | Europe |
| Ireland | 68.5 | 2019 | 357 | 5,235 | 0.068 | 121,496 | Europe |
| Israel | 59.8 | 2019 | 49 | 6,577 | 0.007 | 173,662 | Europe |
| Italy | 53.1 | 2019 | 581 | 4,067 | 0.143 | 107,848 | Europe |
| Japan | 48.0 | 2019 | 8 | 221 | 0.036 | 5,516 | Asia |
| Latvia | 11.7 | 2019 | 16 | 640 | 0.025 | 100,009 | Europe |
| Lithuania | 14.8 | 2019 | 29 | 736 | 0.039 | 182,847 | Europe |
| Luxembourg | 39.8 | 2019 | 179 | 9,665 | 0.019 | 618,326 | Europe |
| Mexico | 82.3 | 2018/2019 | 331 | 2,932 | 0.113 | 6,946 | America |
| Netherlands | 62.7 | 2019 | 358 | 3,077 | 0.116 | 49,709 | Europe |
| New Zealand | 62.0 | 2019 | 4 | 311 | 0.013 | 90,746 | Australia and Ozeanien |
| Norway | 38.2 | 2019 | 47 | 1,677 | 0.028 | 77,531 | Europe |
| Portugal | 60.8 | 2019 | 168 | 4,900 | 0.034 | 149,941 | Europe |
| Romania | 16.1 | 2017 | 112 | 2,272 | 0.049 | 56,571 | Europe |
| Singapore** | 14.0 | 2016/2017 | 5 | 8,523 | 0.001 | 199,896 | Asia |
| Slovak Republic | 12.5 | 2019 | 5 | 392 | 0.013 | 46,285 | Europe |
| Slovenia | 12.9 | 2019 | 55 | 994 | 0.055 | 61,108 | Europa |
| South Korea | 85.1 | 2019 | 6 | 275 | 0.022 | 29,619 | Asia |
| Spain | 54.9 | 2019 | 608 | 6,833 | 0.089 | 135,188 | Europe |
| Sweden | 52.2 | 2019 | 562 | 7,819 | 0.072 | 74,353 | Europe |
| Thailand | 12.0 | 2018/2019 | 0.8 | 47 | 0.017 | 9,817 | Asia |
| Turkey | 7.0 | 2019 | 66 | 2,668 | 0.025 | 53,707 | Europe |
| United Kingdom | 72.0 | 2019 | 673 | 4,398 | 0.153 | 214,532 | Europe |
| United States | 68.7 | 2019 | 450 | 12,929 | 0.035 | 159,672 | America |
| Vietnam*** | 12.0 | 2017 | 0 | 4 | 0.000 | 2,824 | Asia |
To analyze the data, I first calculated the non-parametric Spearman rank correlation coefficient (rs) and its RS2 and respective p-value (2-tailed) to determine any association between DPMI and CFR with IVR, using R (R Core Team, 2017). As the relationship between DPMI and the number of people tested for COVID-19 was not statistically significant based on rs and its p-value, I did not modified (corrected) the DPMI data set. Then, I created regression curves by Generalized additive model (GAM) using the “ggplot2” package and function (method = “gam”) (Wickham, Chang & Wickham, 2013), also in R.
As the analysis included countries with different socioeconomic status, demographic structure, urban/rural settings, time of arrival of the pandemic and national control strategies, there may be complex interactions between IVR and other correlated predictor variables. With the aim of accurately estimating the influence of IVR on DPMI and CFR and mitigating the effects of confounding variables, I performed variable importance ranking, including as predictor variables IVR and some potentially important geographical, socioeconomic and non-pharmaceutical-intervention variables (Escobar, Molina-Cruz & Barillas-Mury, 2020). I used the centroid longitudes (°) and latitudes (°) of each country as geographical variables calculated by the “rgeos” and “rworldmap” packages, along with the “getMap” and “gCentroid” functions, implemented in R (version 3.3.4; R Core Team, 2017). For each country considered, the study recorded socioeconomic variables as the degree of urbanization (DUR) in 2020 (https://www.cia.gov/library/publications/the-world-factbook/fields/349.html), the population density (PD) in 2018 (https://data.worldbank.org/indicator/EN.POP.DNST), the Human Development Index (HDI) in 2018 (http://hdr.undp.org/en/composite/HDI) and the percentage of elderly people (PEP) in 2019 (https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?name_desc=false), which were all retrieved on July 13, 2020 (Table 2). Finally, I recorded two aspects as COVID-19 prevention measures, that is, the degree of requirement to use masks (mask) in public (with three degrees: none, parts of country, full country) (https://masks4all.co/what-countries-require-masks-in-public/) and the lockdown degree (lockdown) (with three levels: no lockdown, partial lockdown, nationwide lockdown); all of these sources and the noted in Table 3 were consulted on Aug 13, 2020.
| Country | Long (°) | Lat (°) | Degree of urbanization (2020)* | HDI (2018)** | Percent elder people (%) (2019)*** | Population density (people per km2 of land area) (2018)**** |
|---|---|---|---|---|---|---|
| Australia | 134.5 | −25.7 | 86.2 | 0.938 | 15.92 | 3.2 |
| Belgium | 4.6 | 50.6 | 98.1 | 0.919 | 19.01 | 377.4 |
| Brazil | −53.1 | −10.8 | 87.1 | 0.761 | 9.25 | 25.1 |
| Canada | −98.3 | 61.4 | 81.6 | 0.922 | 17.65 | 4.1 |
| Chile | −71.4 | −37.7 | 87.7 | 0.847 | 11.88 | 25.2 |
| China | 103.8 | 36.6 | 61.4 | 0.758 | 11.47 | 148.3 |
| Croatia | 16.4 | 45.1 | 57.6 | 0.837 | 20.86 | 73.0 |
| Czech Republic | 15.3 | 49.7 | 74.1 | 0.891 | 19.80 | 137.7 |
| Denmark | 10.0 | 56.0 | 88.1 | 0.930 | 19.97 | 138.0 |
| Estonia | 25.5 | 58.7 | 69.2 | 0.882 | 19.99 | 30.4 |
| Finland | 26.3 | 64.5 | 85.5 | 0.925 | 22.14 | 18.1 |
| France | 2.5 | 46.2 | 81.0 | 0.891 | 20.39 | 122.3 |
| Germany | 15.3 | 49.7 | 77.5 | 0.939 | 21.56 | 237.3 |
| Greece | 23.0 | 39.1 | 79.7 | 0.872 | 21.94 | 83.3 |
| Hungary | 19.4 | 47.2 | 71.9 | 0.845 | 19.69 | 108.0 |
| Ireland | −8.1 | 53.2 | 63.7 | 0.942 | 14.22 | 70.7 |
| Israel | 35.0 | 31.5 | 92.6 | 0.906 | 12.21 | 410.5 |
| Italy | 12.1 | 42.8 | 71.0 | 0.883 | 23.01 | 205.4 |
| Japan | 138.0 | 37.6 | 91.8 | 0.915 | 28.00 | 347.1 |
| Latvia | 24.9 | 56.9 | 68.3 | 0.854 | 20.34 | 31.0 |
| Lithuania | 23.9 | 55.3 | 68.0 | 0.869 | 20.16 | 44.7 |
| Luxembourg | 6.1 | 49.8 | 91.5 | 0.909 | 14.27 | 250.2 |
| Mexico | −102.5 | 23.9 | 80.7 | 0.767 | 7.42 | 64.9 |
| Netherlands | 5.3 | 52.1 | 92.2 | 0.933 | 19.61 | 511.5 |
| New Zealand | 171.5 | −41.8 | 86.7 | 0.921 | 15.99 | 18.4 |
| Norway | 15.3 | 68.8 | 83.0 | 0.954 | 17.27 | 14.5 |
| Portugal | −8.5 | 39.6 | 66.3 | 0.850 | 22.36 | 112.3 |
| Romania | 25.0 | 45.9 | 56.4 | 0.816 | 18.79 | 84.6 |
| Singapore | 103.8 | 1.4 | 100.0 | 0.935 | 12.39 | 7953.0 |
| Slovak Republic | 19.5 | 48.7 | 53.8 | 0.857 | 16.17 | 113.3 |
| Slovenia | 14.8 | 46.1 | 55.1 | 0.902 | 20.19 | 103.0 |
| South Korea | 127.8 | 36.4 | 81.4 | 0.906 | 15.06 | 529.4 |
| Spain | −3.6 | 40.2 | 80.8 | 0.893 | 19.65 | 93.7 |
| Sweden | 16.7 | 62.8 | 88.0 | 0.937 | 20.20 | 25.0 |
| Thailand | 101.0 | 15.1 | 51.4 | 0.765 | 12.41 | 135.9 |
| Turkey | 35.2 | 39.1 | 76.1 | 0.806 | 8.73 | 107.0 |
| United Kingdom | −2.9 | 54.1 | 83.9 | 0.920 | 18.51 | 274.7 |
| United States | −112.5 | 45.7 | 82.7 | 0.920 | 16.21 | 35.7 |
| Vietnam | 106.3 | 16.6 | 37.3 | 0.693 | 7.55 | 308.1 |
Note:
Variable importance ranking was carried out using the “party” package and the non-parametric random forest function “cforest”, along with Out of bag score (with the default option “controls = cforest_unbiased” and the conditional permutation importance “varimp(obj, conditional = TRUE)”). Following the permutation principle of the “mean decrease in accuracy” importance, this machine learning algorithm guarantees unbiased variable importance for predictor variables of different types (Strobl et al., 2008).
To mitigate the effects of confounding factors, IVR, DPMI and CFR evaluations were also conducted for countries with similar social conditions (>50% of DUR, HDI of >0.80, >15% of PEP, and PD between 25 and 350 inhabitants per km2) (Escobar, Molina-Cruz & Barillas-Mury, 2020) and for countries with similar longitudes (10–20° in parts of Europe and 100–140°, East and Southeast Asia along with Australia and New Zealand).
As IVR and the other eight predictor variables were not strongly correlated (|rs| ≤ 0.57; rs (IVR × DUR) = +0.52; rs (IVR × Long) = −0.46; rs (IVR × HDI) = 0.36), therefore, I included these variables in non-parametric Random Forest (RF) models of DPMI and CFR, including a 5-fold cross validation approach, repeated 30 times using the package “caret” together with the function “train” (Venables & Ripley, 1999; Williams et al., 2018, http://topepo.github.io/caret/index.html) in R software. Finally, I evaluated the goodness-of-fit of the regression model using the (pseudo) coefficient of determination (R2) and the root mean square error (RMSE).
Results
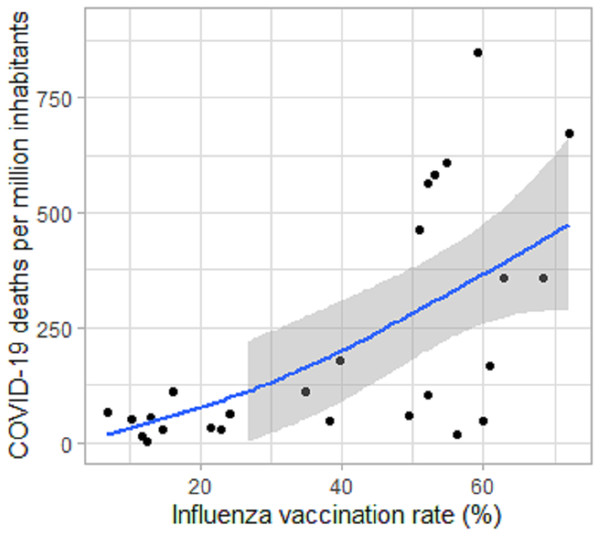
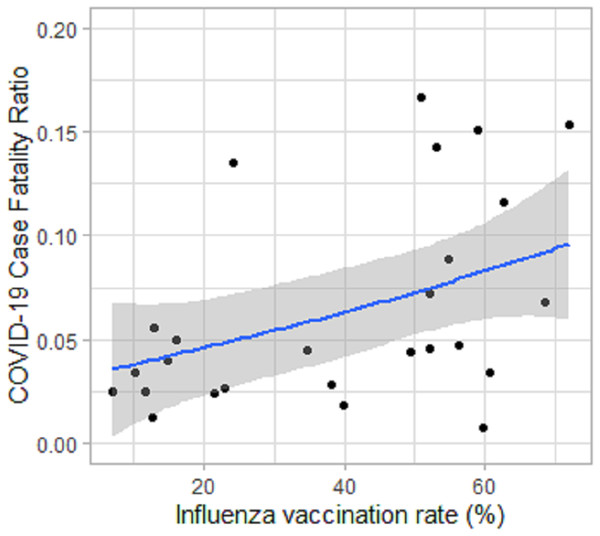
For the 26 European countries considered, the results indicated that COVID-19 DPMI and the COVID-19 CFR were positively and statistically significantly associated with IVR in people ≥65 years-old in 2019 or latest data available (rs (IVR × DPMI) = +0.62 with p = 0.0008, Rs2 (IVR × DPMI) = 0.38; rs (IVR × CFR) = +0.50 with p = 0.01, RS2 (IVR × CFR) = 0.25) (Figs. 1 and 2; Table 4). In evaluations including only countries with similar social conditions, rs (IVR × DPMI) was equal to +0.65 (p = 0.002, N = 20) and rs (IVR × CFR) +0.48 (p = 0.03, N = 20). In analyses including only countries with similar longitude of the country centroid (Long), rs (IVR × DPMI) was equal to +0.83 (p = 0.003, N = 10) (Long from 10° to 20°) and rs (IVR × DPMI) +0.76 (p = 0.046, N = 7) (Long from 100° to 140°).
Figure 1: Association of COVID-19 deaths per million inhabitants (DPMI) up to July 25, 2020 with influenza vaccination rate (IVR) of people aged 65 and older in 2019 or latest data available in Europe.
Association of COVID-19 deaths per million inhabitants (DPMI) up to July 25, 2020 with influenza vaccination rate (IVR) of people aged 65 and older in 2019 or latest data available in Europe (26 countries with more than 0.5 million inhabitants). The mean (blue line) and standard deviation (grey area) are based on generalized additive models (GAM); rs (IVR × DPMI) = +0.687 with p = 0.00015.Figure 2: Association of COVID-19 Case Fatality Ratio (CFR) up to July 25, 2020 with influenza vaccination rate (IVR) of people aged 65 and older in 2019 or latest data available in Europe.
Association of COVID-19 Case Fatality Ratio (CFR) up to July 25, 2020 with influenza vaccination rate (IVR) of people aged 65 and older in 2019 or latest data available in Europe (26 countries with more than 0.5 million inhabitants). The mean (blue line) and standard deviation (grey area) are based on generalized additive models (GAM); rs(IVR × CFR) = +0.629 with p = 0.00075.| var | rs (DPMI × var) | p value |
|---|---|---|
| Long | −0.65 | 0.0003 |
| IVR | 0.62 | 0.0008 |
| DUR | 0.43 | 0.0273 |
| PD | 0.41 | 0.0375 |
| HDI | 0.38 | 0.0533 |
| Lockdown | 0.25 | 0.2146 |
| PEP | −0.07 | 0.7387 |
| Lat (abs) | −0.02 | 0.9313 |
| Mask | 0 | 0.9949 |
Note:
Bold values statistically significant after Bonferroni correction (α = 0.0019).
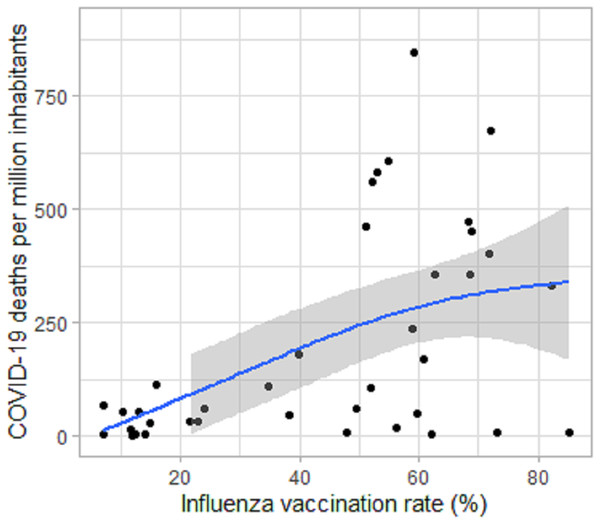
At worldwide level (39 countries studied), the positive associations between DPMI and IVR were also statistically significant (rs (IVR × DPMI) = +0.49 with p = 0.0016, Rs2 (IVR × DPMI) = 0.24) (Fig. 3; Table 5). However, the relationships between IVR and CFR were not statistically significant.
Figure 3: Association of COVID-19 deaths per million inhabitants (DPMI) up to July 25, 2020 with influenza vaccination rate of people aged 65 and older in 2019 or latest data available worldwide.
Association of COVID-19 deaths per million inhabitants (DPMI) up to July 25, 2020 with influenza vaccination rate of people aged 65 and older in 2019 or latest data available worldwide (39 countries with more than 0.5 million inhabitants). The mean (blue line) and standard deviation (grey area) are based on generalized additive models (GAM); rs (IVR × DPMI) = +0.487 with p = 0.0017.| rs | DPMI | CFR |
|---|---|---|
| Long | −0.81 | −0.56 |
| IVR | 0.49 | 0.25 |
| DUR | 0.32 | 0.39 |
| Lat (abs) | 0.32 | 0.03 |
| HDI | 0.20 | 0.10 |
| PEP | 0.15 | 0.38 |
| Mask | 0.14 | −0.01 |
| Lockdown | 0.08 | 0.09 |
| PD | −0.07 | −0.01 |
| p values | ||
| Long | 0 | 0.0002 |
| IVR | 0.0016 | 0.1275 |
| DUR | 0.0436 | 0.8698 |
| Lat (abs) | 0.0451 | 0.0155 |
| HDI | 0.2167 | 0.5529 |
| PEP | 0.3523 | 0.0174 |
| Mask | 0.3819 | 0.9436 |
| Lockdown | 0.6448 | 0.5980 |
| PD | 0.6713 | 0.9347 |
Note:
Bold values statistically significant after Bonferroni correction (α = 0.0019).
In the IVR interval from 7% to 50%, the association was not significant, although a trend for DPMI and CFR to be positively associated with IVR was observed. DPMI and CFR varied strongly when IVR was 50% or higher (Figs. 1–3).
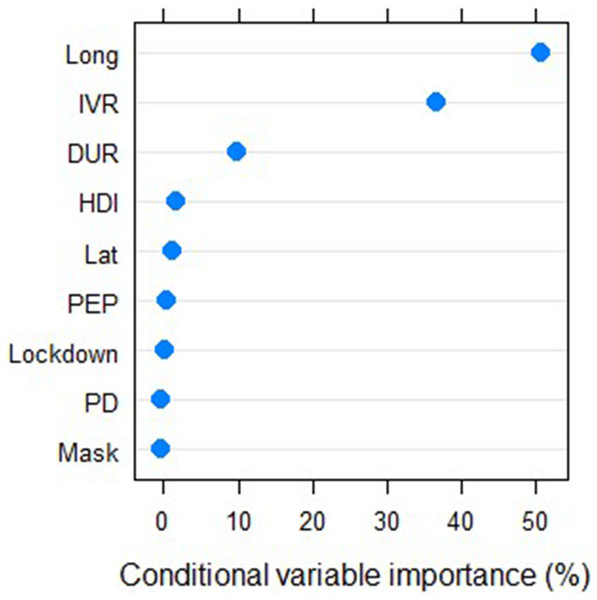
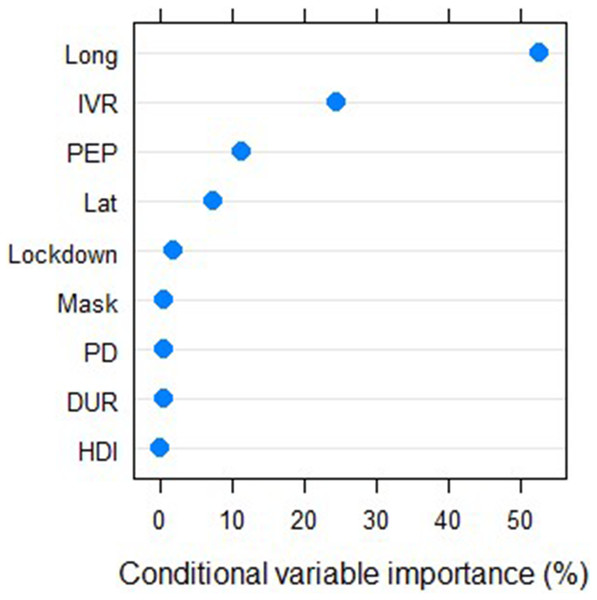
Worldwide, the unbiased ranking showed the degree of importance of each variable analyzed. The variables Long (with 55.9% and 52.3%) and IVR (with 36.3% and 24.5%) were by far the most important of the nine variables used to predict DPMI and CFR, respectively. The DUR in 2020 was the third most important variable, with an importance of 5.7% for predicting DPMI. The PEP in 2019 was the third most important variable (11.5%) in the CFR model (Figs. 4 and 5). The nine predictor variables considered in this study explained 63% of the variation in DPMI (RMSE = 161.9) and 43% of the variation in CFR (RMSE = 0.039).
Figure 4: Unbiased Conditional variables importance ranking to predict COVID-19 deaths per million inhabitant.
Unbiased conditional variables importance ranking (%) to predict COVID-19 deaths per million inhabitants using the package “party” and the non-parametric random forest function “cforest” in the software R; IVR = influenza vaccination rate, Long = centroid longitude (°), Lat = centroid latitude (°), DUR = degree of urbanization in 2020, HDI = Human Development Index in 2018, PEP = percent of elder people in 2019, PD = population density in 2018, mask = the requirement degree of using masks in public (with three degrees: none, parts of country, full country), lockdown = lockdown degree (with three levels: no lockdown, partial lockdown, nationwide lockdown) of each country, at worldwide level (39 countries studied).Figure 5: Conditional variables importance ranking to predict COVID-19 Case Fatality Ratio.
Unbiased conditional variables importance ranking (%) to predict COVID-19 Case Fatality Ratio using the package “party” and the non-parametric random forest function “cforest” in the software R; IVR = influenza vaccination rate, Long = centroid longitude (°), Lat = centroid latitude (°), DUR = degree of urbanization in 2020, HDI = Human Development Index in 2018, PEP = percent of elder people in 2019, PD = population density in 2018, mask = the requirement degree of using masks in public (with three degrees: none, parts of country, full country), lockdown = lockdown degree (with three levels: no lockdown, partial lockdown, nationwide lockdown) of each country, at worldwide level (39 countries studied).Discussion
Contrary to expectations, the present worldwide analysis and European sub-analysis do not support the previously reported negative association between COVID-19 deaths (DPMI) and IVR in elderly people, observed in studies in Brazil and Italy (Fink et al., 2020; Marín-Hernández, Schwartz & Nixon, 2020). Previous studies attributed the beneficial effect of influenza vaccination in reducing severity of COVID-19 disease to better prevention of potential influenza-SARS-CoV-2 coinfections (Arokiaraj, 2020) and, more likely, to changes in innate immunity (Netea et al., 2020). The innate immune response induced by recent vaccination could result in more rapid and efficient SARS-CoV-2 clearance, preventing progressive dissemination into lower areas of lung tissues (Fink et al., 2020).
The negative association between the proportion of DPMI and IVR found in Italy was explained as probably caused by (i) a higher influenza vaccine rate occurring in higher economic groups with overall better health, (ii) chance, (iii) a relationship with seasonal respiratory virus infections, or (iv) an unrelated mechanistic association (Marín-Hernández, Schwartz & Nixon, 2020). However, the induction of cross-neutralizing antibodies and T-cells that directly target other RNA viruses like SARS-CoV-2 and cross-protection seem unlikely, given the extraordinary diversity of influenza viruses (Fink et al., 2020).
Therefore, the above-mentioned arguments cannot explain the positive, direct or indirect relationship between IVR and both DPMI and CFR found in this study, which was confirmed by an unbiased ranking variable importance (Figs. 4 and 5) using RF models. The influenza vaccine may increase influenza immunity at the expense of reduced immunity to SARS-CoV-2 by some unknown biological mechanism, as suggested by Cowling et al. (2012) for non-influenza respiratory virus. Alternatively, weaker temporary, non-specific immunity after influenza viral infection could cause this positive association due to stimulation of the innate immune response during and for a short time after infection (McGill, Heusel & Legge, 2009; Khaitov et al., 2009). People who had received the influenza vaccination would have been protected against influenza but not against other viral infections, due to reduced non-specific immunity in the following weeks (Cowling et al., 2012), probably caused by virus interference (Isaacs & Lindenmann, 1957; Seppälä et al., 2011; Wolff, 2020). Although existing human vaccine adjuvants have a high level of safety, specific adjuvants in influenza vaccines should also be tested for adverse reactions, such as additionally increased inflammation indicators (Petrovsky, 2015) in COVID-19 patients with already strongly increased inflammation (Qin et al., 2020).
The strong variation in DPMI and CFR from an IVR of about 50% or larger may be the result of interactions among the different measures applied in the analyzed countries (Figs. 1–3), for example, initiation of interventions, emergency plans and health systems against COVID-19. For example, Australia and South Korea had a very low DPMI and CFR compared with Belgium and United Kingdom (Table 1).
The high correlation between the longitude of the country centroid and DPMI and CFR emphasize a significant increase in CP and CFR from eastern to western regions in the world (Table 5; Figs. 4 and 5), as confirmed by Leung, Bulterys & Bulterys (2020) and Skórka et al. (2020). Longitude could act as a proxy for variables such as lifestyle, social behavior, genetics, geographically isolated and remote populations, which may also be associated with CP and CFR. In the severe 1918–1919 influenza pandemic, remote or isolated populations were also affected, at least partly because of the lack of prior immunity in locations that had not been recently affected by any form of influenza (Mathews et al., 2009). Therefore, crossing geographical and ecological barriers also is a key factor in spreading diseases (Hallatschek & Fisher, 2014; Murray et al., 2015).
Both DPMI and CFR were weakly and positively correlated (p < 0.05) with the absolute value of geographical latitude (abs(Lat)), DUR, PEP and PD (Tables 4 and 5). In a global analysis, Escobar, Molina-Cruz & Barillas-Mury (2020) also found positive associations between COVID-19 mortality and the percentage of population aged ≥65 years and urbanization, but still more strongly with the Human Development Index. Leung, Bulterys & Bulterys (2020) also reported positive associations between latitude, temperature by week and by month prior to the first reported COVID-19 case. Lower temperature at northern latitudes was a strong independent predictor of national COVID-19 mortality.
Although countywide lockdowns and use of face masks by the general public should reduce COVID-19 transmission (Conyon, He & Thomsen, 2020; Eikenberry et al., 2020), the variables lockdown degree and the degree of requirement for mask use in public were not associated with DPMI and CFR in the present study (Tables 4 and 5; Figs. 4 and 5). Leffler et al. (2020) reported in a global study that internal lockdown requirements were not associated with mortality, but that in countries that recommended use of face masks early on at the national level, the COVID-19 death rate was lower than expected.
Although countywide lockdowns were proclaimed in many countries, the restrictive measures and their implementations differed in degree, strictness and implementation date in relation to the advance of the disease (see references in Table 3). Also, although many countries have required masks in public, the mask quality and correct use may differ from country to country. In this regard, Fischer et al. (2020) found that the use of ineffective masks could be counterproductive. This could explain the non-significant differences between the means of DPMI among countries with and without one or both requirements, lockdown and masks.
Finally, the study is limited by the fact that I didn’t normalize the time of arrival of the pandemic. Moreover, the associations found may change in the future because the COVID-19 pandemic was not over at the end of the study.
Conclusions
Given the positive relationship between IVR and the number of deaths per million found in this study, further exploration would be valuable to explain these findings and to make conclusions. Additional work on this line of research may also yield results to improve prevention of COVID-19 deaths.
Additional Information and Declarations
Competing Interests
Christian Wehenkel is an Academic Editor for PeerJ.
Author Contributions
Christian Wehenkel conceived and designed the experiments, performed the experiments, analyzed the data, prepared figures and/or tables, authored and reviewed drafts of the paper, and approved the final draft.
Data Availability
Funding
The author received no funding for this work.
___

Ei kommentteja:
Lähetä kommentti
You are welcome to show your opinion here!